Introduction to Medical Device PCB Requirements
Medical Device PCB Requirements: Design, Compliance, and Manufacturing Standards Explained
In today’s rapidly evolving healthcare industry, medical device PCB (Printed Circuit Board) technology is foundational to everything from diagnostic imaging systems to life-saving implantables. These boards must meet extremely rigorous functional, regulatory, and reliability standards. At the core of every successful medical device lies not just robust electronics, but precise and compliant PCB design that ensures safety, accuracy, and long-term performance. Understanding medical device PCB requirements is essential for engineers, manufacturers, and developers working to bring reliable and approved medical products to market.
Key Functional Requirements of Medical PCBs
Medical device PCB requirements start with the core function the board is expected to perform. These can include:
- Signal Processing: ECG and EEG devices require high-fidelity signal capture and processing.
- Power Management: Implantables and mobile devices must manage power efficiently with minimal heat.
- Real-Time Data Acquisition: Wearables and diagnostics need immediate data processing and relay.
- Redundancy and Fail-Safe Operation: For life-critical devices, dual-channel systems and watchdog timers are required.
The functional requirements shape the choice of components, layout strategy, and embedded firmware architecture.
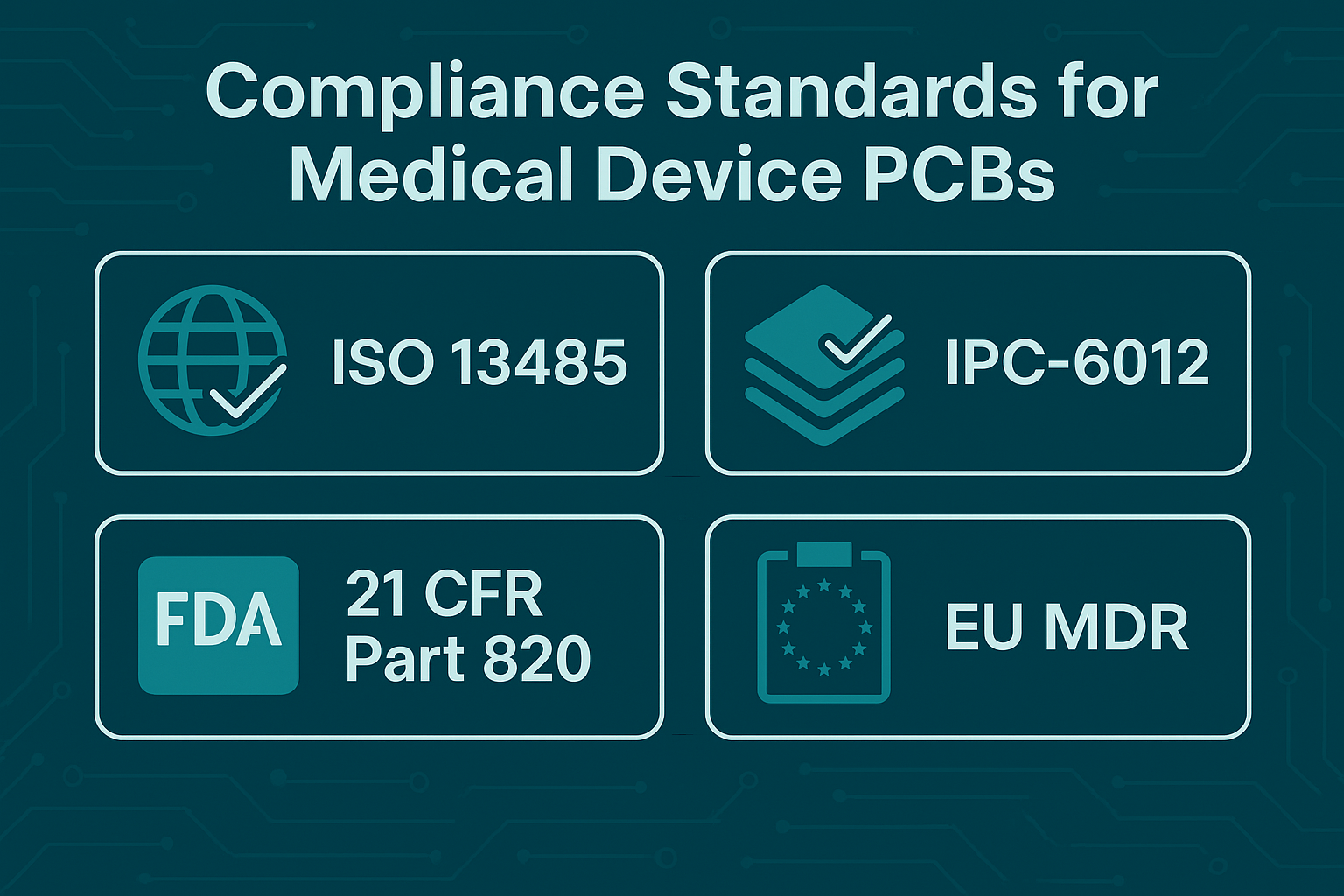
Regulatory and Safety Compliance
FDA (U.S. Food and Drug Administration)
- 21 CFR Part 820 (QSR): Requires design controls, validation, and recordkeeping.
- Premarket Approval (PMA): For high-risk devices, PCB components and manufacturing must be documented and reviewed.
ISO Standards
- ISO 13485: Quality management system requirements for medical device manufacturers.
- ISO 14971: Risk management during the design and manufacture of medical devices.
IEC and UL Standards
- IEC 60601: General safety requirements for medical electrical equipment.
- UL 94: Flame-retardant ratings for PCB materials.
Regulatory compliance is foundational. Any non-conformance can delay approvals, result in product recalls, or pose serious risks to patient health.

Design Standards for Medical Device PCBs
Designing a medical-grade PCB requires close adherence to the following:
1. High-Density and Compact Layout
- HDI (High-Density Interconnect) and Rigid-Flex Designs are essential for implantable or wearable devices.
- Fine Trace Widths: Often 3 mil or less to fit into small geometries.
2. Signal Integrity and EMI/EMC Control
- Shielded traces, ground planes, and isolation zones are mandatory.
- Differential signal pairs are routed for noise immunity.
3. Redundancy
- Dual microcontroller paths or backup batteries may be included.
- Redundant sensors and analog front ends in critical care systems.
4. Design for Test (DFT)
- Add test points and boundary scan support for later verification.
All design choices must be verified with simulations (thermal, signal integrity, EMC) and peer-reviewed for regulatory conformance.
Material and Coating Requirements
Medical device PCB requirements often restrict the materials used to ensure biocompatibility, durability, and reliability:
| Material | Use Case | Notes |
| FR-4 | Diagnostic devices | Economical, non-implantable |
| Polyimide | Flexible and wearable devices | Heat resistant, high reliability |
| Rogers/Ceramic | High-frequency systems (MRI, RF) | Low-loss, high thermal conductivity |
| Parylene Coatings | Implantable PCBs | Biocompatible, moisture barrier |
| ENIG Finish | Implantables, wearables | Flat, corrosion-resistant |
Surface finish matters too: ENIG (Electroless Nickel Immersion Gold) is preferred for solderability and medical-grade reliability.
Environmental and Biocompatibility Considerations
Devices that come into contact with or are implanted in the human body must meet strict environmental and biological standards.
- Cytotoxicity Testing: PCB coatings and materials must not be toxic to cells.
- Sensitization and Irritation Testing: Especially important for skin-worn sensors and monitors.
- Moisture Resistance: Parylene and other conformal coatings are often used to block humidity.
- Corrosion Resistance: Implanted devices need long-term chemical stability inside the human body.
Manufacturing Requirements for Medical PCBs
1. Cleanroom Manufacturing
- Required for class III devices and implants.
- Reduces particulate contamination and maintains sterility.
2. IPC Class 3 Manufacturing
- Highest reliability standards under IPC-6012 Class 3 and IPC-A-600 Class 3.
- Ensures tight control over trace width, solder joints, and via integrity.
3. Process Validation
- IQ, OQ, and PQ (Installation, Operational, and Performance Qualification) protocols must be followed.
4. Equipment Calibration
- All manufacturing and test equipment must be regularly validated and traceable to national standards.
Testing and Validation Protocols
Before a medical PCB can be certified for use, it must undergo:
Functional Testing
- In-circuit testing (ICT) and Boundary Scan.
- Functional testing under real-world load and signal conditions.
Environmental Stress Screening (ESS)
- Includes thermal cycling, vibration, and humidity exposure.
Burn-in Testing
- Devices operate for extended hours under elevated temperatures to detect early failures.
EMC/EMI Testing
- Ensures no interference with other nearby devices (e.g., in hospitals or ICU).
Biocompatibility Validation
- Conducted per ISO 10993 for implantable and body-contacting devices.
All test results must be documented, traceable, and reproducible for audits or regulatory inspections.
Documentation and Traceability Requirements
Robust documentation is one of the most critical medical device PCB requirements. You’ll need:
- Design History File (DHF): All design changes and decisions.
- Device Master Record (DMR): BOM, Gerbers, software, test protocols.
- Device History Record (DHR): Manufacturing data, lot traceability, operator logs.
- Change Control Logs: Engineering Change Orders (ECO) and impact analysis.
All documentation must be backed up, time-stamped, and stored securely for a minimum period (often 10+ years, depending on the region).
Challenges and Best Practices
Common Challenges
- Component obsolescence during long development cycles.
- Balancing miniaturization with reliability.
- Global compliance across multiple regulatory jurisdictions.
Best Practices
✅ Use design and compliance checklists early in the development process.
✅ Engage a certified medical PCB manufacturer with ISO 13485 certification.
✅ Integrate risk management (FMEA) into every design review.
✅ Maintain tight communication between design, QA, and regulatory teams.
Following these practices not only reduces development time but also increases the probability of first-pass regulatory approval.
Conclusion
Meeting medical device PCB requirements is essential to ensure device safety, performance, and regulatory approval. From design and material selection to testing and traceability, each step must adhere to stringent standards set by ISO, FDA, and IEC bodies.
Understanding these requirements from the outset not only protects patient safety but also streamlines the path to market. For engineers, manufacturers, and device innovators, aligning your PCB process with these requirements is the foundation for successful product development in the medical field.
Whether you’re developing a wearable heart monitor, a neural implant, or an advanced diagnostic tool, your journey begins with a deep understanding of medical device PCB requirements.